Current State:
- Montana is number one in the nation for suicides. (Centers for Disease Control)
- Montana is first in the nation per capita for children placed in foster care, currently with
3,900 children in foster care. (MT DPHHS Montana Vital Statistics) - Native Americans in Montana die one full generation ahead of the rest of the population
for both male and female. (MT DPHHS Montana Vital Statistics) - The number of Montana children in foster care has more than doubled since 2011. (MT DPHHS Montana Vital Statistics)
- In 2016, 64 percent were removed from the home for reasons related to parental
substance use. (MT DPHHS Montana Vital Statistics) - Substance Use Treatment is reimbursed by Medicaid at the lowest rate in the four
contiguous states to Montana and those rates have been stagnant for a decade. (Rimrock Comparison Spreadsheet 2019) - Among Medicaid patients, the percentage of infants with perinatal drug exposure
increased from 3.7 percent (2010) to 12.3 percent (2016) and has continued to increase
since 2016. (MT Health Care Foundation Grant 2016 Wrapped in Hope Project – KRMC, St. Joe’s, THS, St. Luke) - An estimated 64,000 Montanans have a substance use disorder. There has been a 427%
increase in meth violations from 2011-2015. 90% of Montanans with Substance Use
Disorder are not receiving treatment. (MT DPHHS Strategic Plan: Interim Draft Report 2017-2019 “Addressing Substance Use Disorder in Montana)
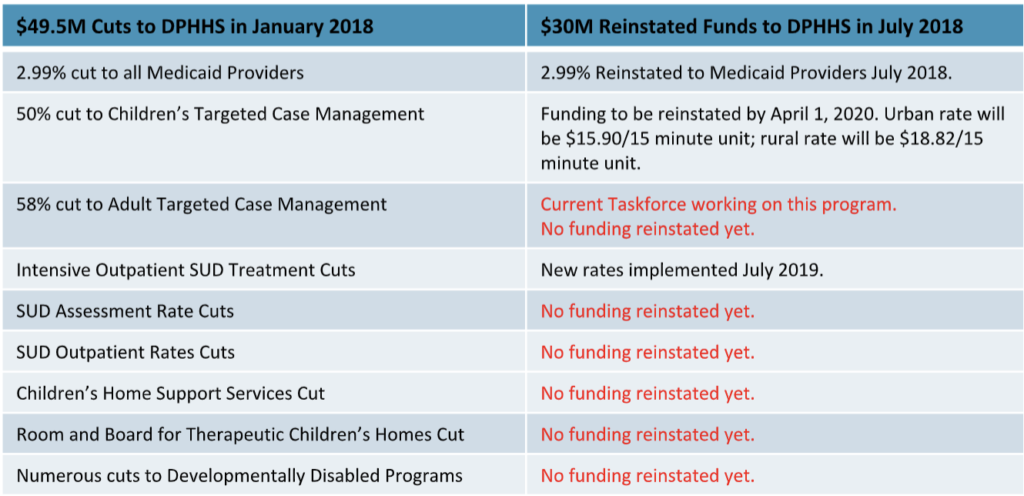
Budget Cuts from 2017 Special Session and Reallocation from July 2018:
The budget cuts from the 2017 special session of the legislature decimated the behavioral health system in Montana. Since that time, multiple behavioral health providers have closed their rural offices and five behavioral health providers have closed their doors completely. The impact across the state to the decimation of prevention programs in behavioral health, such as Home Support Services, Case Management for Adults and Children, Substance Use Assessment Rates, etc., have limited the care available to Montanans.
In addition, the increase of higher paying jobs at community health centers and hospitals, which are reimbursed at substantially higher rates, has limited the number of licensed professionals available to serve the Severely Mentally Ill (SMI) adults and the Severely Emotionally Disabled (SED) children of Montana.
When Home Support Services and children’s case management were cut, many families were left without any resources and were unable to keep their kids at home. Too often, these children go into a higher acuity of care such as a psychiatric residential treatment facility (PRTF) or out of state to a home that has an open bed. Both of these options are considerably more costly and less effective care for the child and families.
When adults with SMI lost their case management, counties saw much higher involuntary commitment rates and higher acuity treatment in more expensive facilities such as hospital behavioral health units (average $2800/day as per Montana State Hospital website) and Montana State Hospital (average $550/day). In Missoula County alone, there was a 30% increase in voluntary commitments (Missoula County Attorney’s Office – involuntary admission data.)
Conclusion:
Until the State of Montana provides strong leadership to address the many challenges to the behavioral health and developmentally delayed individuals and their families in Montana, we
will continue to be number one in everything that holds us back as a state.
With only a million people in Montana, behavioral health providers with strong state leadership
should be able to implement well-known best practices, preventive programs, wrap-around
services, and systems of care for both our children and adults. As long as we continue to fund
the “status quo” in Montana, we will continue to be one of the lowest ranked states in the
nation for the health and well-being of Montanans.
